The term “cloud technology” has come a long way. What once referred to online photo storage or shared business folders has now evolved into something much more powerful – a foundation for innovation across industries, especially healthcare.
In healthcare operations, cloud-based solutions are reshaping how data, workflows, and revenue cycles function. For Revenue Cycle Management (RCM), the cloud isn’t just a storage space – it’s the backbone of agility, accuracy, and scalability.
What is Cloud Computing?
Simply put, cloud computing means accessing and managing data, software, or services through the internet rather than from local servers or physical hardware.
Information and applications are stored online – “in the cloud” – and can be accessed securely by authorized users anytime, anywhere. Security protocols, encryption, and controlled access ensure that data remains safe, even as it flows seamlessly between users and systems.
Cloud computing stands apart from conventional software by offering key advantages:
-
On-demand self-service: Users can access tools and data anytime, without needing manual setup or maintenance.
-
Agility: Updates and improvements roll out instantly across the network.
-
Broad accessibility: Teams can log in from any location using standardized devices.
-
Resource pooling: Multiple users can share and use the same infrastructure efficiently.
-
Rapid scalability: The system adjusts to workload spikes or user growth without downtime.
These traits make cloud computing an ideal fit for healthcare organizations that need fast, reliable, and secure access to data – especially in the realm of revenue cycle management.
What is a Cloud-Based RCM System?
A cloud-based RCM system centralizes all financial, administrative, and billing data in a secure online environment. Unlike traditional RCM software limited by local installations, cloud-based systems connect every part of the revenue cycle – from patient registration to final reimbursement – on a single platform.
This connectivity means updates, automations, and insights are shared across all users in real time. Claims processing, denial management, and payer updates no longer depend on manual interventions or individual servers – they’re managed centrally and intelligently.
Why Cloud-Based RCM Matters
Revenue cycle management depends on accuracy, speed, and adaptability. Cloud-based systems make these possible by:
-
Eliminating silos: Teams across billing, coding, and administration access the same updated data.
-
Enhancing interoperability: Integration with EHRs, clearinghouses, and payers happens smoothly.
-
Reducing IT overhead: There’s no need for heavy infrastructure or manual software installations.
-
Enabling real-time insights: Dashboards and analytics are always current, giving teams visibility into claims, payments, and denials as they happen.
As healthcare shifts toward automation and AI, the cloud offers the agility needed to adapt – ensuring data-driven decision-making and sustainable financial performance.
AI-Driven, Cloud-Native Revenue Cycle Automation
AI is the new catalyst redefining what’s possible in RCM. When combined with a cloud-native architecture, it enables real-time learning across the network – every clean claim, payer update, or denial resolution strengthens the system for everyone connected.
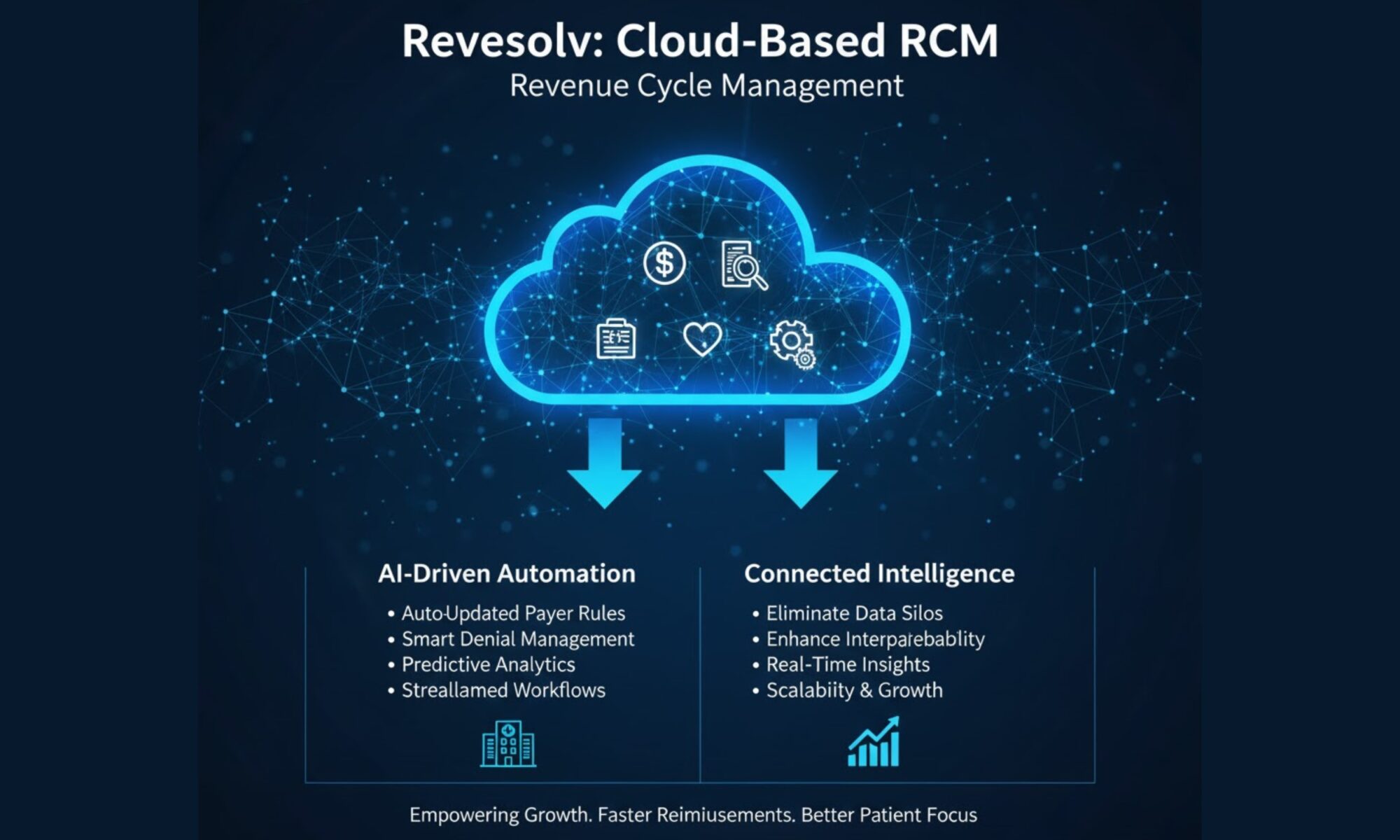
At Revesolv, our cloud-based RCM platform integrates automation and intelligence at every stage of the revenue cycle:
-
Auto-updated payer rules: Every change from payers is reflected instantly across clients.
-
Smart denial management: AI identifies recurring patterns, helping prevent rework and reduce denial rates.
-
Predictive analytics: Algorithms forecast claim outcomes and reimbursement trends before submission.
-
Streamlined workflows: Teams can collaborate in real time, with complete visibility into every claim status.
-
Continuous improvement: The platform learns from each transaction, creating a stronger and more efficient ecosystem over time.
The result? Reduced manual intervention, faster reimbursements, and greater control over financial performance.
Empowering Growth Through Connected Intelligence
Cloud-based RCM isn’t just about technology – it’s about scalability. As practices grow or regulations evolve, cloud-native systems adapt without disruption.
By combining AI-driven intelligence with a centralized, secure, and connected platform, Revesolv empowers healthcare providers and billing teams to focus less on paperwork and more on patients.
The future of RCM is one where automation, transparency, and performance go hand in hand – and with a cloud-based foundation, that future is already here.